The Covid-19 pandemic has accelerated the use of telemedicine across the world. The need to limit the impact of the virus has increased the acceptance of telemedicine by clinicians and patients alike. It looks to have brought about a sustained growth in the use of telemedicine both now and in the future but perhaps it is a little early to tell?
Telemedicine is still in its infancy with regard to the possibilities and potential impact it has to deliver within the healthcare domain. One recent futuristic example of developments of what may become possible and routine with the use of 5G in telemedicine is the recent trial in China of 5G-based remote surgery on the human brain[i].
Increasing availability of 5G technology globally offers telemedicine users a significantly increased bandwidth, reduced latency and greater reliability with which healthcare providers can address the universal challenges of ageing populations, increased patient demand, increasing costs, staff shortages and exponential growth in chronic conditions to a point where it’s estimated that 80% of the cost of healthcare delivery worldwide is due to non-communicable diseases which was pre-pandemic.
5G implementation supplies a far richer and reliable communications environment for telemedicine and will likely play a pivotal role in facilitating the move by healthcare providers to an integrated patient centric model of care which will allow a more preventative and treatment-based healthcare system, and to an interrupt driven appointment system and away from a scheduled system. This will assist in reducing the challenges of fiscal sustainability in healthcare, by automating the routine, facilitating the stratification of patient population on the basis of risk, minimizing the development of acute complications and will result in significantly improving patient outcomes.
To make optimal use of telemedicine we need to address the issue of semantic interoperability in Electronic Healthcare Records (EHRs) such that clinicians have access to a complete unified patient care record summary as well as the alerts and data from smart wearables used to monitor the patient. To achieve this, there needs to be a suite of internationally agreed comprehensive clinical ontologies and terminologies, and whilst there are initiatives around the world, there needs to a single organization to be responsible for this.
Significant progress has been made in the last decade with the development of smart wearables by such companies as Apple, Samsung, Huawei, Dexcom and latterly Amazon as examples. Such devices can measure such vital signs as:
- Blood glucose
- Continuous glucose monitoring
- Blood pressure
- Electrocardiogram (ECG)
- Oxygenetation
- Heart rate
- Sleep pattern
- Acivity
- Temperature
- Mental well-being.
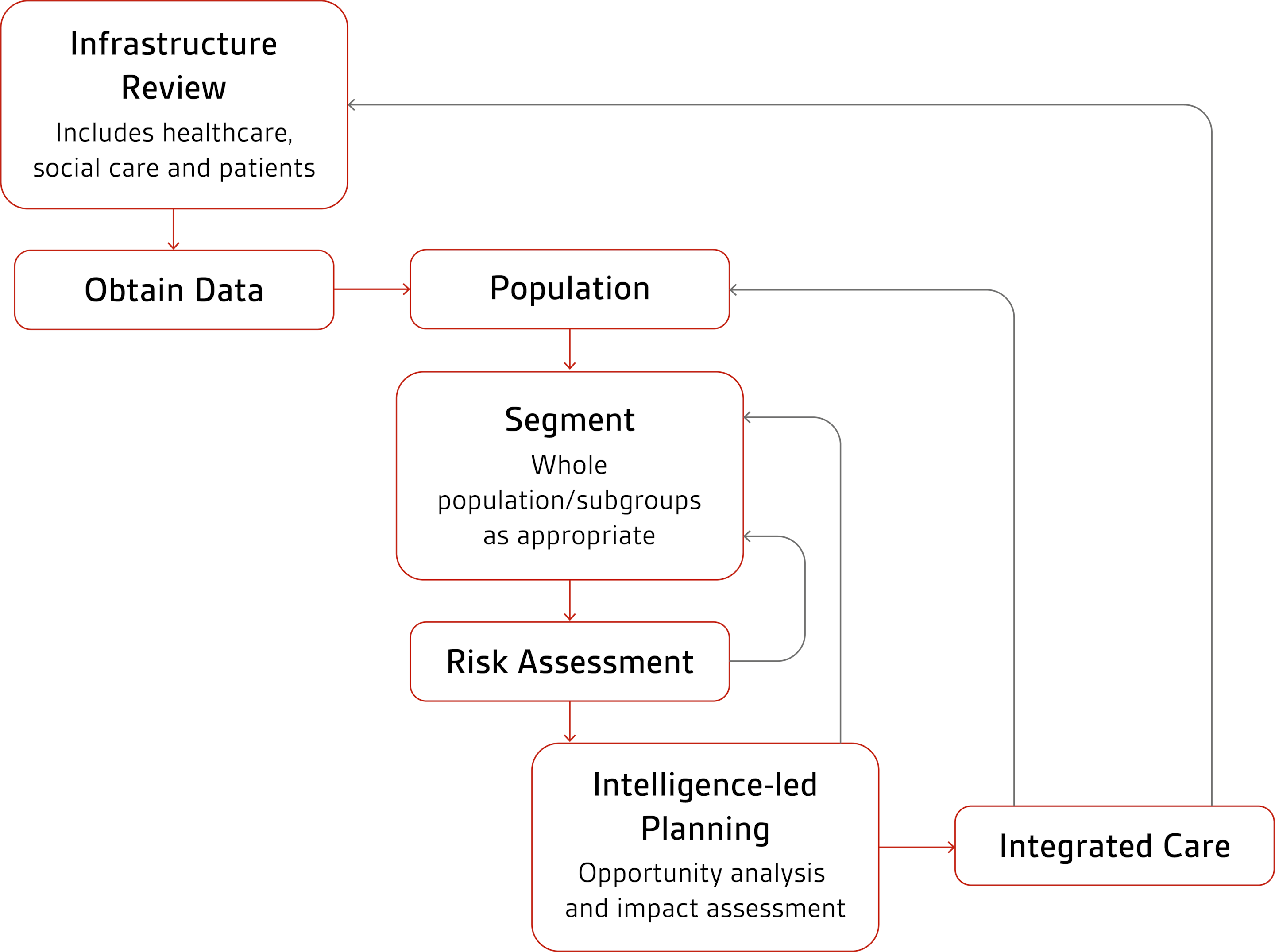
In analyzing and using the data from these wearable devices for telemedicine in the broadest sense, population segmentation is likely to be an important element, that of grouping together individuals within a population into subgroups/segments, based on specific characteristics. For example, patients at the highest risk of the development of acute complications, which can be lifechanging for the patient and a high cost for the provider means that there may be available resources that can be used to reduce such events:
- Separating populations into groups that are clearly differentiated by specific characteristics allows investigation into how each segment interacts with a system and development of strategies tailored according to those characteristics
- The insights obtained help systems and organizations to move away from reactive strategies to those that are both proactive and reactive i.e., those patients most at risk
- The granularity achieved by population segmentation allows predictions and plans to be made that will benefit the specific subgroup and facilitate the goals of more personalized care in healthcare planning.
There is clearly a need for a consistent and efficient single international approval process for wearable devices and associated artificial intelligence (AI).
It’s important that with an ageing population likely to experience comorbidities, monitoring of multiple vital signs is passive from the patient perspective via as few as devices as possible, ideally a single device that’s robust and affordable. To support such a system, patients would need to be able to manage their conditions via a single application and hence a consistent “look and feel”. The entire system to be informed by agreed clinical “best practice”.
In addition, the ecosystem for telemedicine needs high availability and resilience, supports intelligent alert generation that minimizes false positives and false negatives, as well as assists patients with medication management, diet, exercise and mental well-being.
In 2020, the World Health Organization[ii] global strategy on digital health 2020–2025 was endorsed by the 73rd World Health Assembly in decision WHA73(28). With the recognition that information and communications technologies present new opportunities and challenges for the achievement of all 17 UN Sustainable Development Goals, there is growing consensus in the global health community that strategic and innovative use of digital and cutting-edge information and communications technologies will be an essential enabling factor towards ensuring that 1 billion more people benefit from universal health coverage.
Digital transformation of healthcare can be disruptive however, technologies creating a continuum of care have proven potential to enhance health outcomes. These include improving medical diagnosis, data-based treatment decisions, digital therapeutics, clinical trials, self-management of care and person-centered care as well as creating more evidence-based knowledge, skills and competence for professionals to support health care. Examples of technology that creates this continuum of care includes Internet of Things, virtual care, remote monitoring, AI, big data analytics, blockchain, smart wearables, platforms, tools enabling data exchange and storage and tools enabling remote data capture and the exchange of data and sharing of relevant information across the health ecosystem.
Such technology will surely lead to healthcare delivery without borders, huge markets and major benefits for all stakeholders not least for the patient whilst supporting the assertion by Prof. David Cutler - Professor of Applied Economics at Harvard University that “Perhaps the most underused person in healthcare is the patient”.
[i] China Daily - China performs first 5G-based remote surgery on human brain - http://www.chinadaily.com.cn/a/201903/18/WS5c8f0528a3106c65c34ef2b6.html ;
[ii] The World Health Organization - Global strategy on digital health 2020-2025 - https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf