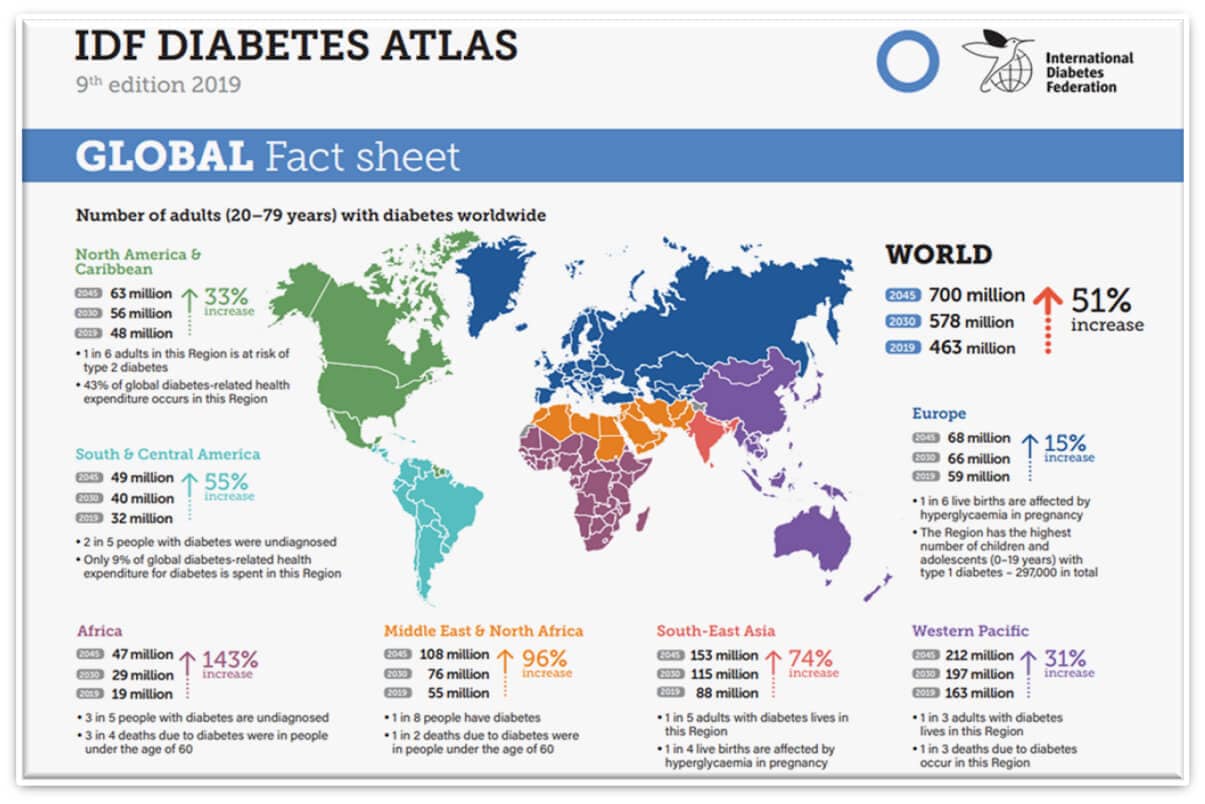
Healthcare systems globally are being challenged continually by demographic changes in population, increased patient demand and expectation, worldwide growth in chronic conditions such as diabetes, and shortages of clinicians and allied staff. This combination of factors is challenging the fiscal sustainability of healthcare services. An example of the growth in just on chronic condition Diabetes (51% by 2045) is shown below [1]:
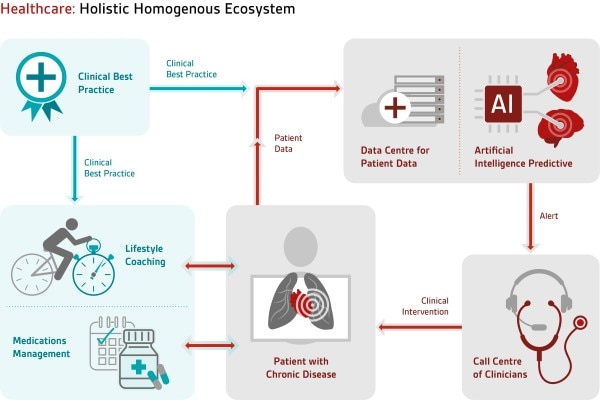
There is a dire need to improve services, reduce unit costs and improve patient outcomes, as well as support the move to a patient centric integrated model of care that is not simply a system that prioritises treatment, but one that can also predict and prevent poor health. Health informatics needs to play an increasing role in the delivery of a more efficient and effective healthcare system. This should include unified summary patient electronic healthcare records and greater use of effective telemedicine systems and healthcare technology. The increased use of data analytics, artificial intelligence (AI) with appropriate ethical and clinical approval, wearable devices and technical standards including standards for clinical ontologies and vocabularies to minimise sematic interoperability problems are examples of fundamental requirements to achieve the necessary transformation of healthcare provision.
It’s widely accepted that the origin of digital health records began with New England Journal of Medicine’s publication by Dr Larry Weed entitled “Medical Records that Guide and Teach” in March of 1968. Over half a century later, no nation has yet delivered a fully integrated unified electronic patient record for its population.
Patient data remains siloed and consequently patient health records are fragmented. Issues of semantic interoperability needs to be resolved going forward and the issues of legacy data need to be addressed. This is a substantial challenge. Failure to resolve these issues delays the creation of an effective integrated care system and the optimal use of eHealth to generate much needed benefits, improved patient outcomes and economies across the domain. Automating the routine whilst enabling limited clinical and nursing resources to be able to address the more complex cases.
In addition to this, there are a number of digital health trends that also need further development. These include but are not limited to:
- improved cybersecurity particularly with the development of quantum computing
- User Role Based Access (RBAC)
- artificial intelligence standards and regulation
- telemedicine
- wearable device approval assisting patients to manage their own conditions
- consistent sources of truth for clinical “best practise” and care pathways
- the use of a common data layer for system integration
- the ability to stratify the patient population on the basis of risk
- standards for the development and use of such technologies as 5G in the provision of healthcare
- development of consistent clinical ontologies and terminologies across the entire healthcare domain
- the effort to ensure that the use of new technologies is affordable and delivers to developing nations the opportunity to ensure structured healthcare is available to their entire populations that do not currently have such.
I will touch on these topics in future blogs that I write but hopefully this gives you some food for thought of where we are at now with digital health trends.
Over the last two decades we have seen a growing adoption in the use of eHealth systems including electronic patient records around the globe. In the last two years the adoption of telemedicine and virtual appointments has seen far greater acceptance, perhaps largely due to the COVID pandemic, this trend is likely to continue.
However, currently whilst patient data often exists in electronic form the data remains siloed or fragmented. In telemedicine the ability to measure patient vital signs during a virtual appointment are limited.
Going forward, my view is that the two greatest challenges in the eHealth domain are the integration of electronic patient records to produce a single electronic summary care record for each patient, and the development of clinical standard affordable wearable devices that measure noninvasively and passively form a patient perspective through a comprehensive range of patient vital signs.
[1] International Diabetes Federation. IDF Diabetes Atlas, 9th edn. Brussels, Belgium: International Diabetes Federation, 2019.